National Centre for Child Trauma and Dissociation
Collaborating on the cutting edge of
research and development.
The members of Integrate have all got a rich heritage working and collaborating in the field of child trauma and dissociation.
Led by Dr Renée P Marks, Integrate has solidified itself as the UK's National Centre of Child Trauma and Dissociation.Renee continues to work in close collaboration with world wide experts in this field
All Integrate therapists work from a trauma and dissociation informed approach and adhere to individual and professional codes of ethics and guidelines, e.g. BACP/ UKCP. Additionally, as specialists working with children and adolescents who have experienced trauma, Integrate Families therapists also refer to the European Society of Trauma and Dissociation, (ESTD) Guidelines for the Assessment and Treatment of Children and Adolescents with Dissociative Symptoms and Dissociative Disorders (2017).
These guidelines, based upon extensive current research and knowledge, state:
Treatment strategies aim to reduce symptoms through increased emotional regulation, effective trauma processing, reduced dissociation and promote integration. The most successful treatment approach to an individual case often is the most eclectic, with the clinician showing flexibility and creativity in the utilisation of a wide variety of available techniques (ISSTD, 2003).
Goals for the treatment of children and adolescents with dissociative symptoms are:
-
To establish safety for the child to the fullest extent possible, to recognize and prevent trauma and reenactments (Ford & Courtois, 2013; Silberg, 2013)
-
To promote stabilization and emotional regulation (Arvidson, Kinniburgh, Howard, Spinazzola, Strothers, Evans, Andres, Cohen, Blaustein, 2011; Silberg, 2013; Struik, 2014).
-
To provide ways for the child to process traumatic experiences (Silberg, 2013; Struik, 2014; Waters, 2016; Wieland, 2015).
-
To establish integration of the dissociative states and enable the child to develop an integrated sense of self. (Silberg, 2013; Struik, 2014; Waters, 2016; Wieland, 2015).
-
To re-integrate the child back in age appropriate levels of functioning across all domains: cognitive, emotional, social and relational. In this way children can develop a sense of agency, competency and mastery over their minds, bodies and lives again (Arvidson et al, 2011; Silberg, 2013; Struik, 2014).
ESTD Guidelines (2017)
The guidelines are in keeping with a phased trauma treatment approach, based upon the three-phased model developed for the treatment of adults (Herman, 1992). The phases are:
-
1. Safety, Stabilisation & Symptom Reduction – the child needs to be stabilised enough to be able to face their traumatic memories and begin trauma processing. This phase includes safety; psychoeducation; attachment work; emotional regulation, internal co-consciousness and co-operation.
-
2.Trauma Processing and working with dissociation - This phase includes externalising the child’s internal world and identifying traumatic memories; the child’s trauma is processed, and dissociative states are identified and Integrated of using a variety of techniques, including EMDR and creative techniques.
-
3. Re-Integration –moving on to age appropriate behaviour; keeping safe; improving social skills; expanding support systems; improving positive self-image; strengthening attachments; building positive experiences.
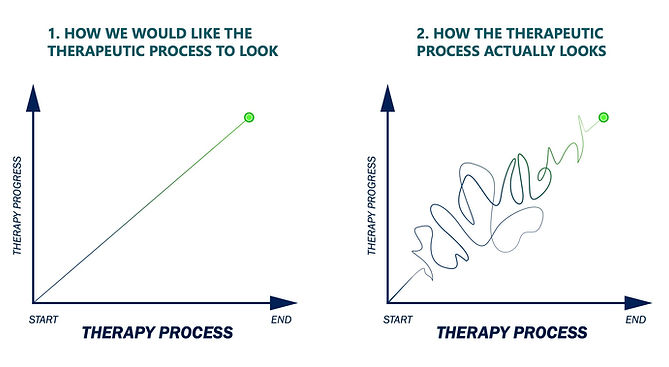
NB the stages do not progress in a neat sequential fashion, e.g. stabilisation occurs throughout therapy. It is difficult to say at the outset, how long therapy may take, as this is dependent upon many factors, including: the timing and duration of the trauma; the child’s pace and motivation, the length of time it takes to achieve safety and stabilisation and parental engagement in the process.
ESTD guidelines state: in terms of length of treatment, “The stabilization phases for children can be very diverse... Age is a strong determining factor…. Children between six and twelve years need some more stabilization, usually several months… Adolescents… stabilization phase can extend to more than one year”.
It may also be that when working with children or adolescents, that the trauma processing may begin earlier in the process, since unlike adults, they are less likely to have developed the degree of avoidant and defensive strategies to the trauma content, that are apparent in traumatised adults (ESTD guidelines 2017)
Assessment:
At Integrate Families, we begin with a thorough, comprehensive clinical assessment of the child’s therapeutic needs, in order to determine the relevant issues. The assessment explores all aspects of the child’s functioning, including cognitive, social, emotional, in addition to identifying any attachment difficulties and the presence of trauma and dissociation.
Phase 1:
Safety and Stabilisation:
In order that therapy has the best chance for success, it’s imperative that the child’s safety needs are currently being met – both physically and emotionally and that an attachment figure is identified who will be integral to the work – both in the therapy room and continuing with work at home. Preparation work and the implementation of a home-based programme, that needs to be done on a daily basis, may also be required to address aspects of the child’s functioning in daily life and to address emotional regulation.
Although many of the children referred to Integrate Families, require therapy if they are to reach their potential, it cannot be assumed that all children and young people will want to access therapy, and we are aware that the older the child, the more difficult it appears to be, for them to engage in the therapeutic process. However, we use multiple ways of assisting the child or young person, with the support of their parents, to engage in the therapy process. This includes psychoeducation and Parent preparation.
Psychoeducation:
Psychoeducation is an educational approach that teaches trauma survivors about different psychological processes and their effects. At Integrate Families, it is important that the child, parents and relevant others e.g. school, receive psychoeducation, in order to make sense of the child’s behaviours, some of which that may appear puzzling and unhelpful. The therapist will explain the effects of trauma and dissociation upon the brain / body, emotions and development and explore strategies that may be helpful to facilitate emotional regulation. It’s often also helpful to explain that the child’s feelings and behaviours are often typical of reactions that other trauma survivors also describe. Understanding these reactions as adaptive ‘survival based’ behaviours at the time of the trauma, but which are impeding the child’s functioning in the present, may help the child and family feel less isolated and blamed. The therapist will also share helpful resources, including, access for the parents to online training, providing information on trauma, attachment and dissociation.
Parent preparation:
Parents are an integral part of the therapy process and Integrate Families value parents’ input and support and aim to work collaboratively with them, in order to help the child or young person. The parents’ own attachment style and possible traumatic experiences and coping strategies are explored in order to enable the parent to be emotionally and psychologically ready, to work alongside the therapist as a co-therapist. Parents will be assisted to see if there is any need to change their parenting style, based upon the assessment information. Parents will also be offered therapy and support to address any secondary or primary trauma that they themselves may have sustained, in the process of parenting their traumatised child.
Phase 2: trauma processing
Trauma processing, in simple terms, is how the child, aided by the therapist, is assisted to externalise their internal world containing the traumatic material, in order to acknowledge and validate the trauma experience. This can then be explored within the safety of the therapeutic relationship and in doing so, can be MADE SENSE OF, before being integrated into the child’s experience. This phase crucially, also involves identifying and working with the child’s dissociative states or parts, resulting from the trauma/s and integrating them, so that the child is no longer fragmented but rather has in integrated, whole sense of self.
During trauma processing, we view the trauma through the eyes of each individual – i.e. each child’s experience is unique. (trauma informed principles). Trauma processing is also informed by neuroscience and the therapeutic input must match the corresponding level of the brain – as in Bruce Perry’s NMT model – Neurosequential Model of Therapeutics.
In other words, in therapy, the trauma experiences are encoded in new ways, which require activation of those areas of the brain originally associated with the trauma. This is undertaken in a safe way, so that the past overwhelming experiences, can be desensitised. In this way, trauma memories are integrated, and new connections are made in the brain.
According to Silberg, (2013), the following components are important to include in the processing of traumatic material with the child survivor:
-
content of the traumatic event (focus on memory of the events),
-
sensorimotor experiences associated with the event,
-
exploring the event’s meaning to the child,
-
affects such as anger, shame, fear, sadness, abandonment and loneliness
-
mastery experiences that counter feelings of powerlessness.
This processing must take place in the context of a validating relationship either with the therapist or: jointly with a loving caregiver.” It’s also important that phase one - safety and stabilisation has been established prior trauma processing, in order to minimize the risk of re-traumatisation.
At Integrate Families, all of our therapists have a therapeutic toolbox that reflects what we work with a variety of children, all of who bring their unique experiences to the therapy room. Each toolbox contains a variety of tools, skills and interventions, that can make use of the child’s strengths and assist them to work with the appropriate brain / body level, in order to access the trauma experience. These include: narrative work, EMDR, sand tray work, play therapies, creative therapies including art and music, sensory work, and body orientated work to name a few.
Trauma therapy is complex and nonlinear work and the staged approach does not always proceed in a neat sequential way, and crucially, stage one – safety and stabilization, is required throughout the therapeutic process.
Phase 3: Re-Integration:
The final phase of therapy – re- integration, involves not only the integration of dissociative parts and processing of the trauma, but re-integration into a world without trauma. This involves the child becoming accustomed to a new way of being, where they are able to function in age appropriate ways in all areas of life.
Here the child may need to assistance to practice newfound skills and to consolidate the gains that they have made throughout the therapeutic process. Resource building, strengthening relationships and support systems and improving social skills are all important during this phase. The aim of completing this final phase as stated in ESTD guideline, is to, “develop a sense of agency, competency and mastery over their minds, bodies and lives again”.
Therapy – practical information.
Therapy usually takes place for 1.5 hours on a weekly basis. There are variations to this based upon practical and clinical information. For example, some children may need to have more frequent sessions in a crisis, or less frequent if nearing the end of the work.
Intensive therapy is also offered, depending upon the child’s needs and subject to funding. This can take place on average for 5 hours per day for 10 days over a 2-week period initially. A further 5 days is undertaken after a period of consolidation of the initial work, (some individual sessions may be required during the consolidation phase and after the intensive is completed). Intensive therapy may also be offered for a lesser number of days, again dependent upon the child’s needs and the available resources.
Therapy is reviewed regularly – at least every six months, and at the review, it is assessed as to which therapy phase the child is in and what is required in order to be able to move to the next phase.
We strive to work in a way that is informed, open and ethical and welcome feedback and questions throughout the therapeutic process.
